Case Study

A 15 year old male had been complaining to his mother of fatigue and a constant thirst. At first the mother suspected him of putting on the symptoms to avoid revising for his exams however when his symptoms apparently worsened and he also started losing weight she became more concerned so took him to their GP. The doctor noted that the boy had been off school the previous year with mumps, having not been immunised as a child but had otherwise been in good health.
What do you think might be the problem with this boy?
The combined symptoms of fatigue, thirst and weight loss and the boy’s age led the GP to suspect that he may have Insulin dependent diabetes mellitus (IDDM). The immune systems of people with IDDM incorrectly produces specifically targeted cells that attack and destroy the islet cells of the pancreas that normally produce insulin, a molecule crucial to the metabolism of sugars. This disease affects around 1 in 3000 people, generally under the age of 30. The cause is uncertain although some people have a genetic predisposition and some researchers in immunology have suggested that infection with a virus, such as mumps or cytomegalovirus, may be a triggering factor.
How might the Doctor investigate whether the patient has Diabetes?

The symptoms and profile of the patient alone are relatively strong indicators for diabetes but several other tests are necessary to make a definitive diagnosis. On referral from the GP, healthcare scientists in the Immunology department used immunofluoresence techniques and found two autoantibodies that are specifically found in patients with diabetes, Islet Cell Antibodies (ICA) and antibodies targeted against a molecule called Glutamic Acid Decarboxylase (GAD). The chemistry department worked on the case alongside the immunology department by measuring blood glucose levels which were found to be high, another strong indication of diabetes. Type 1 diabetes in adolescents is often associated with coeliac disease so clinical scientists in the immunology lab decided to test for antibodies associated with coeliac as a precaution, however these tests were negative.
What do you think might be an appropriate treatment regime for a patient with Diabetes?
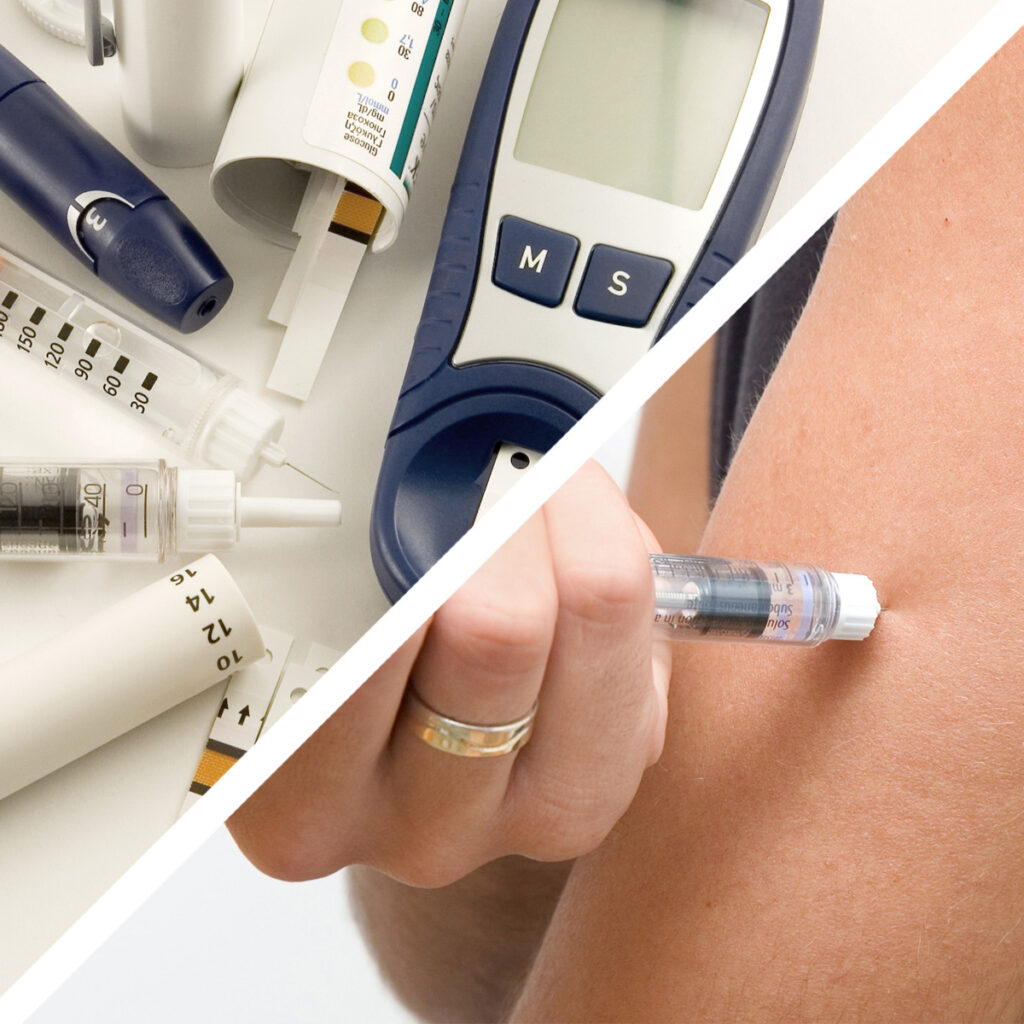
Traditionally this form of diabetes has been controlled by regular self-insulin injections and a carefully controlled diet, so this medication and advice was given to the patient. Young people often have the highest rate of non-compliance with self treatment protocols so the GP advised the family that he would keep them informed of any other possible therapies that might be easier to comply with if they became viable. There are many of these possible solutions currently in research and in clinical trails. New potential treatments include dampening the overactive immune system with specifically directed immunosuppressive drugs and pancreatic or islet cell transplants. As it turns out the patient was relatively disciplined in administering his own injections so was able to rapidly return to a healthy life.
