Background
Tuberculosis (TB) is an important infectious disease in many third world countries but was not considered to be a problem in the UK. A recent upsurge in the number of cases in the UK, partly due to immigration from countries where TB is endemic, has made it a growing concern for the healthcare service. TB infection can be diagnosed by the microbiology department by culturing the organism from patient sputum however this technique is tricky, time consuming and does not always work. Using a cellular assay called an ELISPOT the immunology laboratory can now play a leading role in TB diagnosis. In this test the blood cells are exposed to inactive fragments of TB. This activates the memory cells to secrete proteins that can be measured in the laboratory.
Science
The ELISPOT test is an ‘in vitro’ assay, this means that it recreates an actual biological process in a controlled laboratory environment. In the case of TB diagnosis, we are aiming to recreate an immune response against the TB bacterium that would occur only in people that have a current infection or have had an infection in the past.
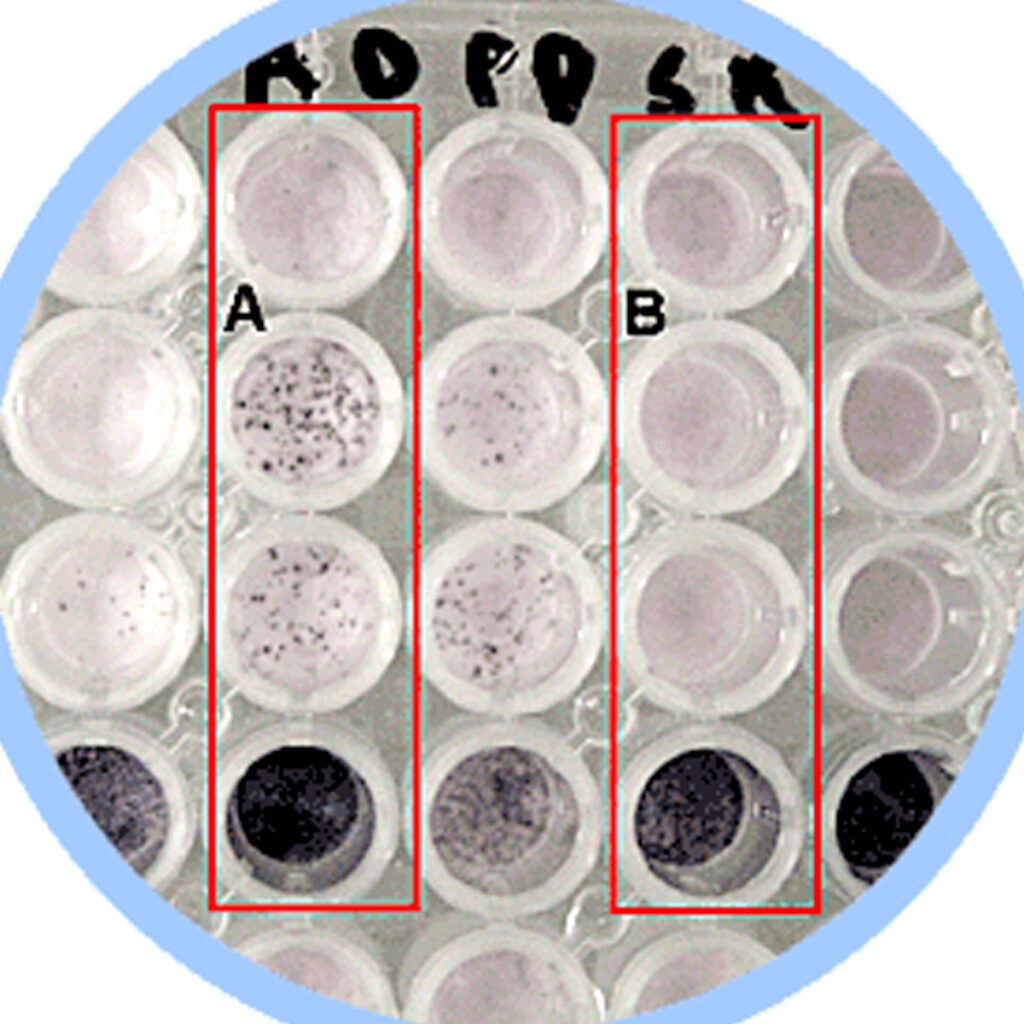
A spinning process called centrifugation separates the lymphocytes (cells responsible for recognition of pathogenic bacteria) from a patient’s blood. These separated cells are mixed with a solution containing specific bacterial proteins (antigens) and incubated for 16-20 hours in a special multi well plate at 37ºC (body temperature). The bottoms of the wells are coated with antibodies that specifically capture a protein called IFN-γ that is released by lymphocytes when they recognise molecules as ‘foreign’. If a patient has been previously exposed to TB, they will have generated a population of lymphocytes that recognise and that are activated by the antigens present in the well. When these cells are activated, they release IFN-γ which becomes trapped by the specific antibodies that are bound to the plate. After the incubation, the cells and antigen mixes are washed off and another antibody, this time one attached to an enzyme, is applied that binds to the trapped IFN-y. After a short incubation, the excess antibody is washed off and then a substance called a substrate is added. The enzymes attached to the antibody cleave the substrate and a coloured precipitate is formed. The final effect is a well that has a number of coloured areas, or “spots” on its base. Each spot indicates the footprint of a cell that has been activated by the TB antigens. The presence of these spots is a strong indication of an active or latent TB infection. Because the outcome of this test could have serious implications for a patient the results are double-checked by the scientist performing the test and by a scientific or medial consultant.
Clinical
TB infection has always posed a significant health problem for the developing world having been brought under control in the developed world. However, due to the increased movement of populations, increasing immunodeficiencies such as HIV infection and emerging drug resistant strains of the TB microorganism, the problem is increasingly considered a global problem. This means that doctors are increasingly more likely to encounter cases in their surgeries and clinics. A doctor may consider investigating a patient for pulmonary TB (the most common form) if he/she presents with symptoms including a prolonged cough, chest pain, haemoptysis (coughing up blood), fever, chills, appetite loss, weight loss and fatigue. The patient would be referred to a specialist clinic where a blood sample would be taken for the immunology laboratory to confirm the diagnosis. Healthcare scientists in the laboratory will perform an ELISPOT test and if a positive result they will contact the TB nurse and clinician to let them know. On receiving the diagnosis the immediate concern is for the patient’s treatment and management so a course of antibiotics would be prescribed. Whereas most bacterial infections often only need a short course of treatment, active TB infection requires a longer period of multiple antibiotic therapy (from 6 to 12 months) to remove the infection completely. To ensure that the patient takes all of his/her medication, the pills are given by a doctor or nurse. This is called DOTS for “direct observation of treatment”. A secondary concern is preventing the spread of infection within the immediate population, the patient’s contacts. This is important if, for example, the patient was attending school. In this case it would be necessary to immediately remove the child from school and to screen their classmates and teachers for the infection.
