Summary
The Polymerase chain reaction (PCR) is a technology originally conceived in the 60’s that enables the user to identify specific DNA, and read the genetic code as well as looking at expression levels of this genetic code. It is considered to have revolutionised many biological fields from forensic pathology to environmental biology. Medical laboratory science has also benefited massively from PCR technology. Virology and some Immunology departmennts use an adaptation of PCR to quantify HIV infection by enabling a count of the viral RNA copy number so that the treatment regimes of patients with the virus can be monitored based on infection level.
Science
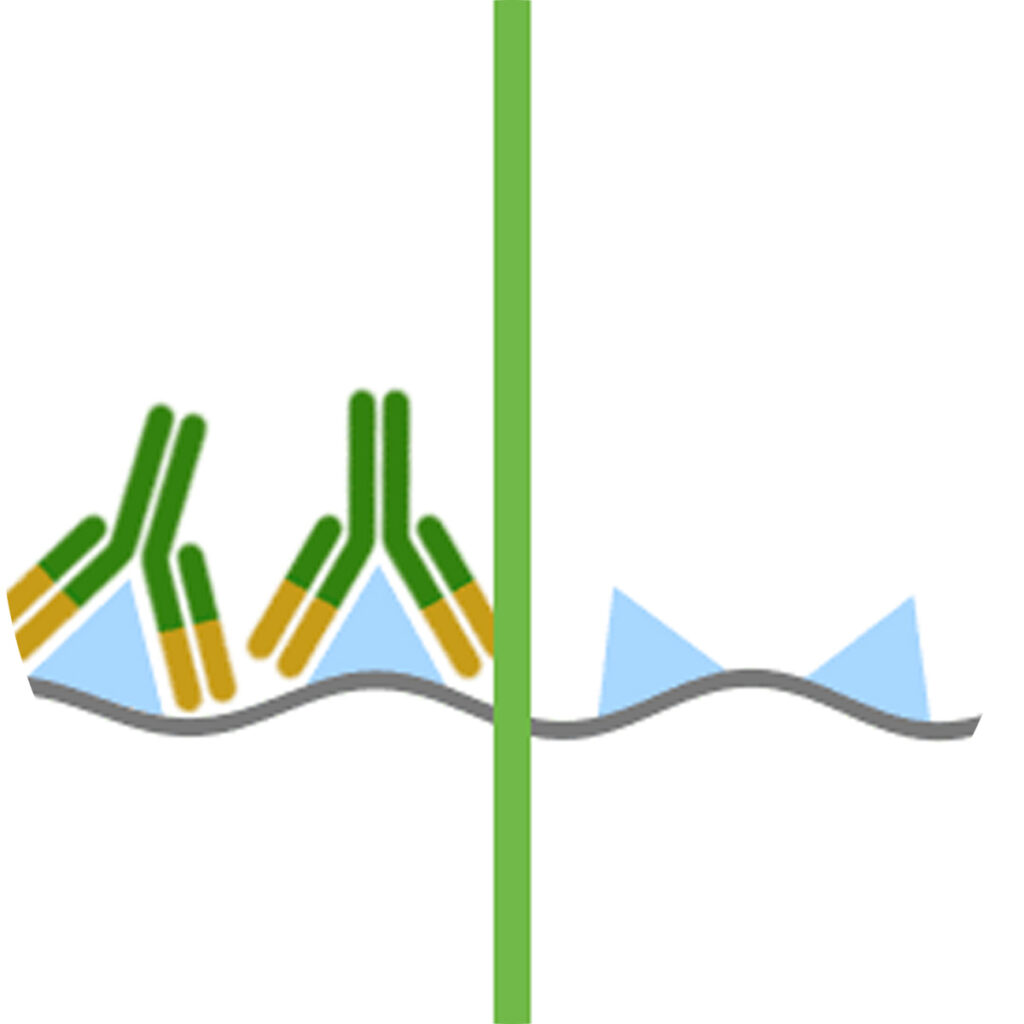
Real time PCR is a quantitative approach to measuring DNA or RNA, this is particularly useful for measuring the viral load present in an infection. Viral RNA is chemically extracted from a patient’s blood sample and is then artificially copied using small artificially produced strands of DNA called primers that are known to be complementary to sections of HIV RNA. When these primers bind to the viral RNA a process that mimics cellular RNA replication is initiated ultimately resulting in millions of copies of the original target sequence. At the same time fluorescent probes are added that also bind specifically to the viral DNA. The increasing amount of fluorescence can be measured over time and compared with fluorescence from samples with known starting concentrations of a non-infectious artificial viral construct. In this was the fluorescence at certain time points can be attributes to an actual viral load.
Clinical

It is important to note that real time PCR plays no role in the initial diagnosis of HIV infection. Once a diagnosis has been made by other techniques, usually carried out in a virology department, viral load as determined by rtPCR becomes extremely important in monitoring disease progress. The viral load of a patient has a direct consequence on the number of functional CD4 T cells present because these are the cells in which the virus replicates and ultimately destroys. CD4 cells are crucial immune components in clearing infections so when they are depleted the individual gradually become more immunocompromised and more likely to get infections and other complications that are known as AIDS defining illnesses. At these late stages of HIV infection it becomes very hard to retain low viral load levels. After an initial burst in the virus population with initial infection the numbers generally drop to low levels in patients on anti-retroviral therapy so after this individuals routinely have their viral load tested every 3 to 6 months. If a clinician notices that some time after the initial HIV infection the viral load has destabilised and is increasing from acceptable levels, they may need to change the anti-viral therapy that the patient is on to prevent depletion of CD4 cell populations.
Monitoring technologies like this and improvements in drug regimes have partly contributed to the greatly enhanced life expectancy of an HIV infected individual over the last 20 years.
